Insomnia theme by Stevie Klym
Download: Insomnia.p3t

(4 backgrounds)
| Insomnia | |
|---|---|
| Other names | Sleeplessness, trouble sleeping |
 | |
| Depiction of insomnia from the 14th century medical manuscript Tacuinum Sanitatis | |
| Pronunciation | |
| Specialty | Psychiatry, sleep medicine |
| Symptoms | Trouble sleeping, daytime sleepiness, low energy, irritability, depressed mood[1] |
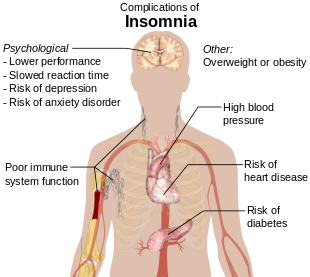
| Complications | Motor vehicle collisions[1] |
| Causes | Unknown, psychological stress, chronic pain, heart failure, hyperthyroidism, heartburn, restless leg syndrome, others[2] |
| Diagnostic method | Based on symptoms, sleep study[3] |
| Differential diagnosis | Delayed sleep phase disorder, restless leg syndrome, sleep apnea, psychiatric disorder[4] |
| Treatment | Sleep hygiene, cognitive behavioral therapy, sleeping pills[5][6][7] |
| Frequency | ~20%[8][9][10] |
Insomnia, also known as sleeplessness, is a sleep disorder where people have trouble sleeping.[1] They may have difficulty falling asleep, or staying asleep for as long as desired.[1][9][11] Insomnia is typically followed by daytime sleepiness, low energy, irritability, and a depressed mood.[1] It may result in an increased risk of accidents of all kinds as well as problems focusing and learning.[9] Insomnia can be short term, lasting for days or weeks, or long term, lasting more than a month.[1] The concept of the word insomnia has two possibilities: insomnia disorder (ID) and insomnia symptoms, and many abstracts of randomized controlled trials and systematic reviews often underreport on which of these two possibilities the word insomnia refers to.[12]
Insomnia can occur independently or as a result of another problem.[2] Conditions that can result in insomnia include ADHD, psychological stress, chronic pain, heart failure, hyperthyroidism, heartburn, restless leg syndrome, menopause, certain medications, and drugs such as caffeine, nicotine, and alcohol.[2][8] Other risk factors include working night shifts and sleep apnea.[9] Diagnosis is based on sleep habits and an examination to look for underlying causes.[3] A sleep study may be done to look for underlying sleep disorders.[3] Screening may be done with two questions: "do you experience difficulty sleeping?" and "do you have difficulty falling or staying asleep?"[9]
Although their efficacy as first line treatments is not unequivocally established,[13] sleep hygiene and lifestyle changes are typically the first treatment for insomnia.[5][7] Sleep hygiene includes a consistent bedtime, a quiet and dark room, exposure to sunlight during the day and regular exercise.[7] Cognitive behavioral therapy may be added to this.[6][14] While sleeping pills may help, they are sometimes associated with injuries, dementia, and addiction.[5][6] These medications are not recommended for more than four or five weeks.[6] The effectiveness and safety of alternative medicine is unclear.[5][6]
Between 10% and 30% of adults have insomnia at any given point in time and up to half of people have insomnia in a given year.[8][9][10] About 6% of people have insomnia that is not due to another problem and lasts for more than a month.[9] People over the age of 65 are affected more often than younger people.[7] Women are more often affected than men.[8] Descriptions of insomnia occur at least as far back as ancient Greece.[15]
Signs and symptoms[edit]
Symptoms of insomnia:[17]
- Difficulty falling asleep, including difficulty finding a comfortable sleeping position
- Waking during the night, being unable to return to sleep and waking up early
- Not able to focus on daily tasks, difficulty in remembering
- Daytime sleepiness, irritability, depression or anxiety
- Feeling tired or having low energy during the day[18]
- Trouble concentrating
- Being irritable, acting aggressive or impulsive
Sleep onset insomnia is difficulty falling asleep at the beginning of the night, often a symptom of anxiety disorders. Delayed sleep phase disorder can be misdiagnosed as insomnia, as sleep onset is delayed to much later than normal while awakening spills over into daylight hours.[19]
It is common for patients who have difficulty falling asleep to also have nocturnal awakenings with difficulty returning to sleep. Two-thirds of these patients wake up in the middle of the night, with more than half having trouble falling back to sleep after a middle-of-the-night awakening.[20]
Early morning awakening is an awakening occurring earlier (more than 30 minutes) than desired with an inability to go back to sleep, and before total sleep time reaches 6.5 hours. Early morning awakening is often a characteristic of depression.[21] Anxiety symptoms may well lead to insomnia. Some of these symptoms include tension, compulsive worrying about the future, feeling overstimulated, and overanalyzing past events.[22]
Poor sleep quality[edit]
Poor sleep quality can occur as a result of, for example, restless legs, sleep apnea or major depression. Poor sleep quality is defined as the individual not reaching stage 3 or delta sleep which has restorative properties.[23]
Major depression leads to alterations in the function of the hypothalamic–pituitary–adrenal axis, causing excessive release of cortisol which can lead to poor sleep quality.
Nocturnal polyuria, excessive night-time urination, can also result in a poor quality of sleep.[24]
Subjectivity[edit]
Some cases of insomnia are not really insomnia in the traditional sense, because people experiencing sleep state misperception often sleep for a normal amount of time.[25] The problem is that, despite sleeping for multiple hours each night and typically not experiencing significant daytime sleepiness or other symptoms of sleep loss, they do not feel like they have slept very much, if at all.[25] Because their perception of their sleep is incomplete, they incorrectly believe it takes them an abnormally long time to fall asleep, and they underestimate how long they stay asleep.[25]
Problematic digital media use[edit]
In August 2018, Sleep Science and Practice published a systematic review and meta-analysis of 19 studies comprising 253,904 adolescent subjects that found that excessive technology use had a strong and consistent association with reduced sleep duration and prolonged sleep onset latency for adolescents 14 years of age or older.[26] Also in August 2018, Sleep Science published a systematic review of 12 studies investigating associations between exposure to video games, sleep outcomes, and post-sleep cognitive abilities that found the data present in the studies indicated associations between a reduction in sleep duration, increased sleep onset latency, modifications to rapid eye movement sleep and slow-wave sleep, increased sleepiness and self-perceived fatigue, and impaired post-sleep attention span and verbal memory.[27] In October 2019, Sleep Medicine Reviews published a systematic review and meta-analysis of 23 studies comprising 35,684 subjects that found a statistically significant odds ratio for sleep problems and reduced sleep duration for subjects with internet addiction.[28] In February 2020, Psychiatry Research published a systematic review and meta-analysis of 14 studies that found positive associations between problematic smartphone use and poor sleep quality and between higher levels of problematic smartphone use and elevated risk of poor sleep quality.[29]
Also in February 2020, Sleep Medicine Reviews published a systematic review of 31 studies examining associations between screen time and sleep outcomes in children younger than 5 years and found that screen time is associated with poorer sleep outcomes for children under the age of 5, with meta-analysis only confirming poor sleep outcomes among children under 2 years.[30] In March 2020, Developmental Review published a systematic review of 9 studies that found a weak-to-moderate association between sleep quantity and quality and problematic smartphone use among adolescents.[31] In October 2020, the International Journal of Environmental Research and Public Health published a systematic review and meta-analysis of 80 studies that found that greater screen time was associated with shorter sleep duration among toddlers and preschoolers,[32] while the Journal of Behavioral Addictions published a systematic review and meta-analysis of 40 studies with 33,650 post-secondary student subjects that found a weak-to-moderate positive association between mobile phone addiction and poor sleep quality.[33] In April 2021, Sleep Medicine Reviews published a systematic review of 36 cross-sectional studies and 6 longitudinal studies that found that 24 of the cross-sectional studies and 5 of the longitudinal studies established significant associations between more frequent social media use and poor sleep outcomes.[34]
In June 2021, Frontiers in Psychiatry published a systematic review and meta-analysis of 34 studies comprising 51,901 subjects that established significant associations between problematic gaming and sleep duration, poor sleep quality, daytime sleepiness, and other sleep problems.[35] In September 2021, BMC Public Health published a systematic review of 49 studies investigating associations between electronic media use and various sleep outcomes among children and adolescents 15 years of age or younger that found a strong association with sleep duration and stronger evidence for an association with sleep duration between the ages of 6 and 15 years than for 5 years of age or younger, while evidence for associations between electronic media use with other sleep outcomes was more inconclusive.[36] In December 2021, Frontiers in Neuroscience published a systematic review of 12 studies published from January 2000 to April 2020 that found that adult subjects with higher gaming addiction scores were more likely to have shorter sleep quantity, poorer sleep quality, delayed sleep timing, and greater daytime sleepiness and insomnia scores than subjects with lower gaming addiction scores and non-gamer subjects.[37] In January 2022, Early Childhood Research Quarterly published a systematic review and meta-analysis of 26 studies that found a weak but statistically significant association with increased smartphone and tablet computer use and poorer sleep in early childhood.[38]
In May 2022, the Journal of Affective Disorders published a meta-analysis of 29 studies comprising 20,041 subjects that found a weak-to-moderate association between mobile phone addiction and sleep disorder and that adolescents with mobile phone addiction were at higher risk of developing sleep disorder.[39] In August 2022, the International Journal of Environmental Research and Public Health published a systematic review and meta-analysis of 16 studies comprising 8,077 subjects that established a significant association between binge-watching and sleep problems and a stronger association between binge-watching and sleep problems was found during the COVID-19 pandemic than pre-pandemic.[40] In October 2022, Reports in Public Health published a systematic review of 23 studies that found that excessive use of digital screens by adolescents was associated with poor sleep quality, nighttime awakenings, long sleep latency, and daytime sleepiness.[41] In December 2022, Sleep Epidemiology published a systematic review of 18 studies investigating associations between sleep problems and screen time during COVID-19 lockdowns that found that the increased screen time during the lockdowns negatively impacted sleep duration, sleep quality, sleep onset latency, and wake time.[42] In March 2023, the Journal of Clinical Sleep Medicine published a systematic review and meta-analysis of 17 studies comprising 36,485 subjects that found that smartphone overuse was closely associated with self-reported poor sleep quality, sleep deprivation, and prolonged sleep latency.[43]
In April 2023, Sleep Medicine Reviews published a systematic review of 42 studies that found digital media use to be associated with shorter sleep duration and poorer sleep quality and bedtime or nighttime use with poor sleep outcomes, but only found associations for general screen use, mobile phone use, computer and internet use, internet, and social media and not for television, game console, and tablet use.[44] In July 2023, Healthcare published a systematic review and meta-analysis of 16 studies that established a correlation coefficient of 0.56 between nomophobia and insomnia.[45] In September 2023, PLOS One published a systematic review and meta-analysis of 16 studies of smartphone addiction and sleep among medical students found that 57% of subjects had poor sleep and 39% of subjects had smartphone addiction with a correlation index of 0.3,[46] while Computers in Human Behavior published a meta-analysis of 23 longitudinal studies comprising 116,431 adolescent subjects that found that adolescent screen time with computers, smartphones, social media, and television are positively associated with negative impacts on sleep health later in life.[47]Causes[edit]
While insomnia can be caused by a number of conditions, it can also occur without any identifiable cause. This is known as Primary Insomnia.[48] Primary Insomnia may also have an initial identifiable cause, but continues after the cause is no longer present. For example, a bout of insomnia may be triggered by a stressful work or life event. However the condition may continue after the stressful event has been resolved. In such cases, the insomnia is usually perpetuated by the anxiety or fear caused by the sleeplessness itself, rather than any external factors.[49]
Symptoms of insomnia can be caused by or be associated with:
- Sleep breathing disorders, such as sleep apnea or upper airway resistance syndrome[50]
- Use of psychoactive drugs (such as stimulants), including certain medications, herbs, caffeine, nicotine, cocaine, amphetamines, methylphenidate, aripiprazole, MDMA, modafinil, or excessive alcohol intake[51]
- Use of or withdrawal from alcohol and other sedatives, such as anti-anxiety and sleep drugs like benzodiazepines[51]
- Use of or withdrawal from pain-relievers such as opioids[51]
- Heart disease[52]
- Restless legs syndrome, which can cause sleep onset insomnia due to the discomforting sensations felt and the need to move the legs or other body parts to relieve these sensations[53]
- Periodic limb movement disorder (PLMD), which occurs during sleep and can cause arousals of which the sleeper is unaware[54]
- Pain:[55] an injury or condition that causes pain can preclude an individual from finding a comfortable position in which to fall asleep, and can also cause awakening.
- Hormone shifts such as those that precede menstruation and those during menopause[56]
- Life events such as fear, stress, anxiety, emotional or mental tension, work problems, financial stress, birth of a child, and bereavement[53]
- Gastrointestinal issues such as heartburn or constipation[57]
- Mental, neurobehavioral, or neurodevelopmental disorders such as bipolar disorder, clinical depression, generalized anxiety disorder, post traumatic stress disorder, schizophrenia, obsessive compulsive disorder, autism, dementia,[58]: 326 ADHD,[59] and FASD
- Disturbances of the circadian rhythm, such as shift work and jet lag, can cause an inability to sleep at some times of the day and excessive sleepiness at other times of the day. Chronic circadian rhythm disorders are characterized by similar symptoms.[51]
- Certain neurological disorders such as brain lesions, or a history of traumatic brain injury[60]
- Medical conditions such as hyperthyroidism[2]
- Abuse of over-the-counter or prescription sleep aids (sedative or depressant drugs) can produce rebound insomnia[51]
- Poor sleep hygiene, e.g., noise or over-consumption of caffeine[51]
- A rare genetic condition can cause a prion-based, permanent and eventually fatal form of insomnia called fatal familial insomnia[61]
- Physical exercise: exercise-induced insomnia is common in athletes in the form of prolonged sleep onset latency[62]
- Increased exposure to the blue light from artificial sources, such as phones or computers[63]
- Chronic pain[64][65]
- Lower back pain[65]
- Asthma[65]
Sleep studies using polysomnography have suggested that people who have sleep disruption have elevated night-time levels of circulating cortisol and adrenocorticotropic hormone.[66] They also have an elevated metabolic rate, which does not occur in people who do not have insomnia but whose sleep is intentionally disrupted during a sleep study. Studies of brain metabolism using positron emission tomography (PET) scans indicate that people with insomnia have higher metabolic rates by night and by day. The question remains whether these changes are the causes or consequences of long-term insomnia.[67]
Genetics[edit]
Heritability estimates of insomnia vary between 38% in males to 59% in females.[68] A genome-wide association study (GWAS) identified 3 genomic loci and 7 genes that influence the risk of insomnia, and showed that insomnia is highly polygenic.[69] In particular, a strong positive association was observed for the MEIS1 gene in both males and females. This study showed that the genetic architecture of insomnia strongly overlaps with psychiatric disorders and metabolic traits.
It has been hypothesized that epigenetics might also influence insomnia through a controlling process of both sleep regulation and brain-stress response having an impact as well on the brain plasticity.[70]
Substance-induced[edit]
Alcohol-induced[edit]
Alcohol is often used as a form of self-treatment of insomnia to induce sleep. However, alcohol use to induce sleep can be a cause of insomnia. Long-term use of alcohol is associated with a decrease in NREM stage 3 and 4 sleep as well as suppression of REM sleep and REM sleep fragmentation. Frequent moving between sleep stages occurs with; awakenings due to headaches, the need to urinate, dehydration, and excessive sweating. Glutamine rebound also plays a role as when someone is drinking; alcohol inhibits glutamine, one of the body's natural stimulants. When the person stops drinking, the body tries to make up for lost time by producing more glutamine than it needs. The increase in glutamine levels stimulates the brain while the drinker is trying to sleep, keeping them from reaching the deepest levels of sleep.[71] Stopping chronic alcohol use can also lead to severe insomnia with vivid dreams. During withdrawal, REM sleep is typically exaggerated as part of a rebound effect.[72]
Benzodiazepine-induced[edit]
Like alcohol, benzodiazepines, such as alprazolam, clonazepam, lorazepam, and diazepam, are commonly used to treat insomnia in the short-term (both prescribed and self-medicated), but worsen sleep in the long-term. While benzodiazepines can put people to sleep (i.e., inhibit NREM stage 1 and 2 sleep), while asleep, the drugs disrupt sleep architecture: decreasing sleep time, delaying time to REM sleep, and decreasing deep slow-wave sleep (the most restorative part of sleep for both energy and mood).[73][74][75]
Opioid-induced[edit]
Opioid medications such as hydrocodone, oxycodone, and morphine are used for insomnia that is associated with pain due to their analgesic properties and hypnotic effects. Opioids can fragment sleep and decrease REM and stage 2 sleep. By producing analgesia and sedation, opioids may be appropriate in carefully selected patients with pain-associated insomnia.[55] However, dependence on opioids can lead to long-term sleep disturbances.[76]
Risk factors[edit]
Insomnia affects people of all age groups but people in the following groups have a higher chance of acquiring insomnia:[77]
- Individuals older than 60
- History of mental health disorder including depression, etc.
- Emotional stress
- Working late night shifts
- Traveling through different time zones[11]
- Having chronic diseases such as
